Table of Contents
- What Is a Vasectomy?
- Common Myths About Vasectomy
- The Procedure Step by Step
- Recovery and Aftercare
- Risks and Benefits
- Vasectomy and Masculinity
- Long-Term Considerations
- Resources and Support
What Is a Vasectomy?
A vasectomy is a medical procedure designed to offer men a permanent birth control solution. Specifically, the vas deferens—small tubes that carry sperm from the testicles to the urethra—are either cut or sealed to prevent sperm from entering the semen. It means that when a man ejaculates, the semen will not contain sperm, making pregnancy virtually impossible. Vasectomy is considered a minor, outpatient surgical procedure that requires only local anesthesia in most cases. It can be done in a urologist’s office or a clinic setting. Recovery is generally quick compared to other surgical procedures.
For those seeking more information or wishing to consult experts before making a decision, clinics such as https://goldenstateurology.com/locations/fremont/ offer accessible educational resources and professional guidance. According to data from the Centers for Disease Control and Prevention, vasectomy is among the most reliable forms of contraception worldwide. It is chosen by approximately half a million men in the United States each year. With a track record spanning decades, vasectomy continues to be endorsed by medical professionals as a highly effective and low-risk option for those seeking long-term contraception.
Common Myths About Vasectomy
Despite its widespread use, many myths about vasectomy persist, causing unnecessary anxiety and confusion. A common fear is that vasectomy will interfere with a man’s ability to enjoy sex, as some believe it might decrease libido, alter orgasm, or lead to erectile dysfunction. However, scientific research consistently demonstrates that vasectomy does not affect testosterone production, sexual desire, or performance. The surgery targets only the pathway for sperm, leaving all sexual function and sensation intact. Post-procedure, semen still looks and feels the same, as sperm constitutes only a tiny fraction of the ejaculate.
Another persistent myth is that vasectomy is always reversible. While reversal procedures, known as vasovasostomy, can sometimes restore fertility, their chances of success decrease significantly the longer the interval since the initial vasectomy. Costs for such reversals can be substantial, and they are not always covered by health insurance. Men who remain unsure about their family plans are encouraged to discuss options like sperm banking and possible future desires with a healthcare provider before proceeding. It’s better to view vasectomy as a lifelong decision rather than an easily undone procedure.
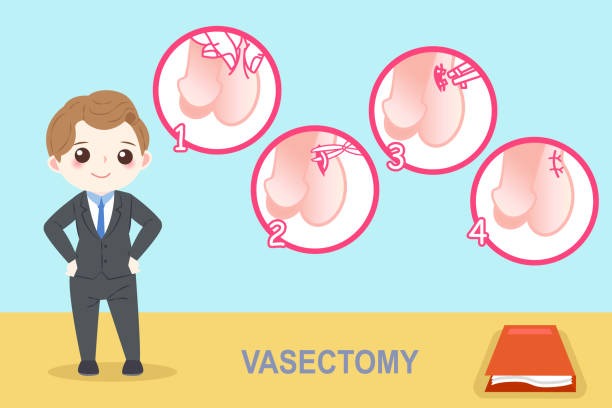
The Procedure Step by Step
- Consultation: This vital first step involves a thorough examination of the patient’s medical history and a meaningful discussion about family planning expectations. During the consultation, all questions regarding risks, benefits, and recovery are addressed, and both personal considerations and technical expertise guide the decision-making process.
- Preparation: On the day of the procedure, the patient is typically asked to shower and shave the area as directed. In the clinic, the scrotal area is sterilized, and a local anesthetic is administered to numb the region and ensure comfort during the entire process.
- Surgical Process: The surgeon makes a tiny puncture or one or two small incisions in the scrotum, gently pulling out each vas deferens. The tubes are cut and either sealed or clamped and then placed back. Afterward, the openings are closed, often without stitches. Several advanced techniques, such as the “no-scalpel” method, further minimize discomfort and expedite recovery.
- Post-Procedure: Immediately after, patients are monitored briefly for any complications before heading home the same day. The entire surgical process often takes less than 30 minutes, with most men describing only mild discomfort rather than significant pain.
Some patients find it helpful to arrange for a friend or family member to drive them home. Aftercare instructions are provided to help encourage prompt and comfortable healing, and a follow-up appointment is usually scheduled to confirm all is well.
Recovery and Aftercare
Early recovery from a vasectomy is typically swift. Most men notice some mild swelling, slight bruising, or a dull ache in the scrotum, but this usually fades within a few days. There are steps patients can take for optimal healing:
- Apply ice packs to the area for several hours to reduce swelling.
- Wear tight-fitting briefs or an athletic supporter to keep the area stable and minimize discomfort.
- Rest and avoid standing as much as possible during the first day. Refrain from strenuous work and vigorous exercise for at least a week.
- Take only the pain relief prescribed or recommended by the doctor, avoiding medications that can increase bleeding risk.
Sex and ejaculation should be postponed according to medical advice, typically for about a week, to prevent complications and ensure complete healing. Men should remember that vasectomy is not immediately effective—semen samples must be tested after several ejaculations to make sure sperm are no longer present. It’s critical to use an alternative form of contraception until a doctor confirms sterility.
Risks and Benefits
Vasectomy promises a straightforward, permanent solution for birth control, but like all procedures, it comes with benefits and some risks. The primary benefit is its extremely high success rate—over 99% effective, meaning only a handful of pregnancies occur among thousands of couples after a correctly performed vasectomy. Compared to tubal ligation (female sterilization), vasectomy is less invasive, requires less recovery time, and carries fewer medical risks.
Minor risks include swelling, mild pain, bruising, and infection, all of which are rare and typically resolve with simple treatments. Even less frequently, chronic pain or granuloma (a lump due to leaking sperm) may develop. Very rarely, tubes may rejoin, allowing sperm through and leading to potential fertility. Most side effects resolve on their own, and severe complications are exceptional. According to this comprehensive summary by WebMD, the overall satisfaction rate for vasectomy is very high, and regret rates are low among men who are certain of their decision.
Vasectomy and Masculinity
A major roadblock for some men is the mistaken belief that undergoing a vasectomy undermines masculinity or impacts sexual prowess; however, medical evidence tells a different story. Vasectomy does not change hormone levels, muscle mass, body hair, or sex drive. The organs responsible for producing testosterone—the testicles—are untouched, so there’s no loss in strength, vitality, or ability.
Many couples find their intimacy improves without the anxiety of accidental pregnancy. Openly discussing these concerns with a healthcare provider or counselor can help clarify any confusion, reduce anxiety, and provide reassurance, allowing you to feel confident and informed about making decisions. Coreassurance
The permanency of a vasectomy is both its strength and its challenge. While it frees men from ongoing concerns over contraception, it also requires deep consideration. Family situations can change unexpectedly due to relationship changes, personal loss, or changes in relationships. Therefore, men are encouraged to discuss all possibilities and even consider a cooling-off period after making the decision but before scheduling the procedure.
Some opt for emergency banking before the procedure as a safeguard, but this does not guarantee late utility payments. Reviewing all long-term factors helps ensure that no future regret complicates what should be a relieving and empowering step toward family planning.
Resources and Support
Deciding on a vasectomy can feel daunting, but access to trustworthy resources and social support can make the process significantly easier. Men are encouraged to read patient testimonials, consult frequently asked questions, and seek out reputable information from leading organizations, such as the CDC’s contraception page. Family discussions and conversations with a supportive healthcare provider remain critical throughout the process.
Online communities or men’s health forums also offer a wealth of personal experiences and practical tips, helping to reduce stigma and provide reassurance at all stages of the journey. Taking the time to ask questions, gather facts, and lean on available support helps make vasectomy a positive and empowered choice for many.